Introduction
Patients who have received an allogeneic stem cell transplant (allo-HSCT) and require acute care in the intensive care unit (ICU) are unlike other patients requiring ICU care. The use of current ICU-based prognostic indices (APACHE II, SAPS II, and SOFA) have not shown to be useful for patients who have received an allo-HSCT. In order to better understand this patient population, we retrospectively analyzed patient, disease and hospital specific factors to determine if there were any risks that had significant prognostic value.
Methods
Data was collected from 413 patients undergoing allogeneic stem cell transplant at a single center from 2007-2013. Of the patients analyzed, 52 patients required ICU support during their HSCT admission. Of these patients the median age at time of transplantation was 59 (range: 26-75) with 52% male and 48% female. The indications for HSCT were: AML (42%), NHL (12%), ALL (10%), MM (10%), MDS (12%), CLL (10%), CML (2%), HD (2%) and AA (2%). The HSCT donor types were: matched-unrelated (56%), double cord (12%), matched-related (33%), and syngeneic. For these patients we reviewed and analyzed several variables, including age, performance status, HCT-CI, DRI, neutrophil engraftment status. The low range for HCT-CI was defined as 0-1 (52%), the moderate-high range 2+ (48%). Median time to neutrophil engraftment was 15 days (9-36 days).
Results
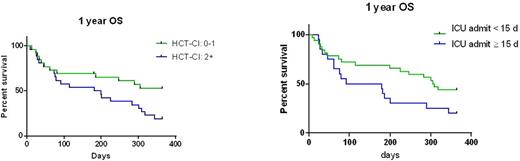
Our multivariate analysis revealed that HCT-CI and timing of ICU admission (pre or post-engraftment) where significant prognostic factors. Allo-HSCT patients requiring ICU support with a low HCT-CI score had a significantly better 1 year overall survival in comparison to similar patients with moderate to high HCT-CI scores (p=0.04). We also found that allo-HSCT patients requiring ICU support after neutrophil engraftment (>15 days) had a worse 1 year overall survival compared to HSCT patients requiring ICU prior to neutrophil engraftment (p= 0.04).
Conclusion
There is a great need for more specific prognostic factors for allo-HSCT patients requiring ICU support. Our findings demonstrate the potential utility of the HCT-CI and timing of ICU admission in the outcomes of HSCT patients admitted to the ICU. Based on these findings we plan to explore these factors in a larger prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.